What is Bronchiectasis?
Bronchiectasis is a condition in which there is an abnormal widening of one or more airways. This may include damage to the airway walls causing them to widen and become flabby and scarred or damage to the cilia (hairs which move the mucus up the airway walls).
Causes
The cause of bronchiectasis is often not clear. Some conditions that affect or damage airways can cause the disease, for example:
- Some inherited conditions. For example, a condition called primary ciliary dyskinesia affects the cilia, so they do not 'move' correctly to clear the mucus. Cystic fibrosis is another condition that affects the lungs and causes bronchiectasis.
- Inhaled objects can become stuck and block an airway. This may lead to local damage to that airway. Acid from the stomach that is regurgitated and inhaled can damage airways as well as inhaling poisonous gases.
- Severe lung infections such as tuberculosis (TB), whooping cough, pneumonia or measles can damage the airways at the time of infection. Bronchiectasis may then develop.
- Pollution and Smoke. It has been found that smoke and certain pollutants affect the development the cilia in the airways, reducing or stopping their growth and causing issues with cilia function. This is particularly the case for children in their lung development stages.
- Old Age. As we grow past the age of 45 years old, the airways start to lose their elasticity and collagen, similar to our skin on the outside of our body, affecting the airway walls and cilia.
What Does This Mean for someone with Bronchiectasis?
In order to fully understand the effects of damage to the airway walls and cilia, the mucus secretory and mucociliary function need to be discussed first. Mucus is the body’s first line of defence against airway tissue damage from breathing in irritants, such as soot, particle matter, dust, microbes and smoke (See Figure 2).
When smaller air particles pass through the nose or mouth and reach the bronchi and bronchioles (airways or the lungs), the mucus that lines the airways catches most of these particles and the cilia (tiny hairs) moves the mucus upward and out into the throat, where it is either swallowed or coughed up and spat out. Elimination of the particles from the lungs plays a large role in preventing permanent damage of lung function and development of lung diseases.
How Does Damage to the Cilia or Airway Walls Effect This Process?
Among other factors severe air pollutants, such as vehicle exhaust and cigarette smoke, contain toxic compounds which have the potential to reduce the airway’s ability to form new cilia (the tiny hairs in the airways which assist the lungs to remove of mucus and pollutants from the body).
Damage to the airway walls and/or cilia can create trenches in the mucociliary escalator, which in turns traps the mucus and stops it from being transported up to the throat to be swallowed or cleared naturally.
This contaminated mucus becomes trapped and can lead to further inflammation, causing an endless loop of infection, inflammation and excess mucus creation, which can lead to further obstruction to the airways causing further breathing difficulties.
How Does This Affect Bronchiectasis?
Defects of the cilia may cause prolonged exposure of individuals to harmful airborne particulate matter, occupational dusts, traffic exhaust and tobacco smoke. This also leads to the development of 2 major conditions similar to effects of smoking and development of Emphysema and Chronic Bronchitis:
- Air Trapping (See Figure 3) is when the airways leading to the air sacs become blocked up when breathing out, so the oxygen (O2) can go into the air sac for gas exchange, but the carbon dioxide (CO2) can’t escape. The air flows into the air sac (alveoli), but can’t escape, causing a build-up in pressure and may lead to damage of the air sac.
- Collapsed Lungs from mucus plugging (See Figure 4) are where the airways are fully closed due to the build-up of mucus in the airways, leading to a full plug being stuck in the airways, stopping air from entering and exiting the air sac. Because air can’t escape from the air sac, the lungs absorb the CO2 from the air sac through the blood stream and move it to another air sac which can then release this gas. The air sac remains collapsed and is no longer used.
Medication is used to relieve inflammation, but it can’t release the trapped air or the mucus plugs which cause the air sac to remain blocked. 2 studies have found a decline in lung function of between 44 to 64 millilitres per year. This is equivalent to more than 1-2 shot glass every year or over 4 shot glasses every 2 years (See Figure 5).
What can you do to help your lungs?
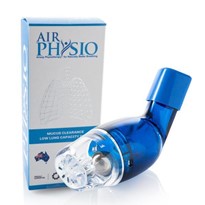
Bronchiectasis can’t be changed unless the lung tissue or cilia can be repaired. Some things which can change include keeping as active as possible as this will help some of these conditions. A key component which will help a number of these processes is the use of Oscillating Positive Expiratory Pressure (OPEP) devices like AirPhysio.
AirPhysio is a mucus clearance and lung expansion device designed to assist in the body’s natural mucus clearance process and improving lung hygiene by performing 3 key functions:
- Wind sheering of the mucus – This is when the air rushes over the mucus and mobilises the top layer of mucus to be breathed or coughed out naturally, helping to reduce the amount/weigh of the mucus in the lungs,
- PEP – The device creates a Positive Expiratory Pressure (help inflate the lungs while breathing out) in the lungs, helping to open up the airways, getting in behind the mucus and helping to push the mucus up and out of the lungs,
- Oscillation – The device vibrates the walls of the airways in the lungs by inflating and deflating the airways at between 15 to 35 times per second, helping to shake the walls, improving the mobilisation of the mucus and helping to clear out the built-up congestion.
The device also helps to reduce trapped air in the lungs and remove mucus plugs, which may be caused by the cold or flu, expanding the lungs and assisting to restore maximum lung capacity. The device is designed to assist conditions like Emphysema, Bronchiectasis and Asthma which create obstructions in the airways and can lead to air trapping and collapsed lungs.
References
- National Heart, Lung and Blood Institute (n.d.). What is Bronchiectasis? Retrieved from https://www.nhlbi.nih.gov/health-topics/bronchiectasis
- World Health Organization (n.d.). Chronic respiratory diseases: Retrieved from http://www.who.int/respiratory/other/bronchiectasis/en/
- Berend, N. (2016). Contribution of air pollution to COPD and small airway dysfunction. Respirology (Carlton, Vic.), 21(2), 237-244. doi:10.1111/resp.12644
- Rogers, D. F. (2007). Physiology of airway mucus secretion and pathophysiology of hypersecretion. Respiratory Care, 52(9) 1134-1149. Retrieved from http://rc.rcjournal.com/content/respcare/52/9/1134.full.pdf
- Rubin, B. K. (2014). Secretion properties, clearance, and therapy in airway disease. Published in Translational Respiratory Medicine, 109, 297-307. doi:10.1186/2213-0802-2-6
- Möller, W., Häußinger, K., Ziegler-Heitbrock, L., & Heyder, J. (2006). Mucociliary and long-term particle clearance in airways of patients with immotile cilia. Respiratory Research, 7(10), 1-8. doi:10.1186/1465-9921-7-10
- Brown, J. S., Zeman, K. L. & Bennett, W. D. (2002). Ultrafine particle deposition and clearance in the healthy and obstructed lung. American Journal of Respiratory and Critical Care Medicine, 166, 1240–1247. doi:10.1164/rccm.200205-399OC
- Crotta, S., Ahlfors, H., Dingwell, K., & Smith, J. C. (2016). The aryl hydrocarbon receptor controls cyclin O to promote epithelial multiciliogenesis. Nature Communications, 1-11. doi:10.1038/ncomms12652
- Kumar, R., Shadie, A., Bucknall, M., Rutlidge, H., Garthwaite, L., Herbert, C.,… Wark, P. (2015). Differential injurious effects of ambient and traffic-derived particulate matter on airway epithelial cells. Respirology, 20, 73-79. doi: 10.1111/resp.12381
- Roth, M. (2015). Airway and lung remodelling in chronic pulmonary obstructive disease: A role for muscarinic receptor antagonists? Drugs, 75, 1-8. doi: 10.1007/s40265-014-0319-0
- Kulkarni, N., Pierse, N., Rushton, L., & Grigg, J. (2006). Carbon in airway macrophages and lung function in children. The New England Journal of Medicine, 355(1), 21-30
- Gauderman, W. J., Vora, H., McConnell, R., Berhane, K., Gilliland, F., Thomas, D.,… Kunzli, N. (2007). Effect of exposure to traffic on lung development from 10 to 18 years of age: a cohort study. Lancet, 369, 571–77. doi:10.1016/S0140-6736(07)60037-3
- AstriMedbø, HasseMelbye. Lung function testing in the elderly—Can we still use FEV1/FVC<70% as a criterion of COPD? Respiratory Medicine. https://doi.org/10.1016/j.rmed.2006.11.019
- Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference values from a sample of the general U.S. population. Am J Respir Crit Care Med. 1999 Jan;159(1):179-87. http://www.atsjournals.org/doi/full/10.1164/ajrccm.159.1.9712108
- Hirofumi Tanaka, Douglas R. Seals. Endurance exercise performance in Masters athletes: age-associated changes and underlying physiological mechanisms. The Journal of Physiology DOI: 10.1113/jphysiol.2007.141879 http://onlinelibrary.wiley.com/doi/10.1113/jphysiol.2007.141879/full
- Kuhlman JE1, Reyes BL, Hruban RH, Askin FB, Zerhouni EA, Fishman EK, Siegelman SS. Abnormal air-filled spaces in the lung. Radiographics. 1993 Jan;13(1):47-75. http://pubs.rsna.org/doi/pdf/10.1148/radiographics.13.1.8426936
- Morsch, A.L., Amorim, M. M., Barbieri, A., Santoro, L. L., & Fernandes, A.L. (2008). Influence of oscillating positive expiratory pressure and the forced expiratory technique on sputum cell counts and quantity of induced sputum in patients with asthma or chronic obstructive pulmonary disease. Jornal Brasileiro De Pneumologia : Publicacao Oficial Da Sociedade Brasileira De Pneumologia E Tisilogia, 34(12), 1026-32.
- Myers, T. (2007). Positive expiratory pressure and oscillatory positive expiratory pressure therapies. Respiratory Care, 52(10), 1308-1327
- Sharma Gulshan and Goodwin James. Effect of aging on respiratory system physiology and immunology. Clin Interv Aging. 2006 Sep; 1(3): 253–260. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2695176/
- Tom Fardon , Simon M. Finch , Megan Crichton , Alison J. Dicker , Sara Marshall , James D. Chalmers. Identifying Modifiable Risk Factors for Rapid Lung Function Decline in Bronchiectasis. AM j Respir Crit Med 193;2016:A2878. https://www.atsjournals.org/doi/pdf/10.1164/ajrccm-conference.2016.193.1_MeetingAbstracts.A2878