The Forgotten Condition of Asthma
Whenever someone has an asthma attack, three events occur:
- Bronchoconstriction – The muscles around the airways tighten, strangling the airways making it harder to breathe.
- Inflammation of the soft tissue - The soft tissue inside of the airways become inflamed causing the airways to narrow further making it harder to breathe.
- Excess Mucus Release – A large amount of sticky mucus is released in to airways clogging them up and making it even harder to breathe.
At this point, everyone grabs for their reliever medication, the muscles around the airways relax and the inflammation is reduced, but the mucus is still stuck in the airways, because this mucus has special properties which make it harder to clear.
"For over 100 years, pathologists have recognized the primary role diffuse mucus plugging play in the pathophysiology of asthma. However, many clinicians do not recognize and treat mucus dysfunction in patients with asthma, possibly because cough in asthma is often unproductive and therapies for asthma focus mainly on reversing bronchoconstriction and inflammation, thereby resulting in unavailability of therapies to clear mucus plugs in asthma.”
The New England Journal of Medicine, 363(23), 2233-2247. 10. Fahy, J. V. & Dickey, B. F. (2010). Airway mucus function and dysfunction.
What happens if this mucus isn’t cleared from the lungs?
- Air Trapping - is when the airways leading to the air sacs become blocked up when breathing out, so the oxygen (O2) can go into the air sac for gas exchange, but the carbon dioxide (CO2) can’t escape. The air flows into the air sac (Aveoli), but can’t escape, causing a build-up in pressure and may lead to damage of the air sac.
- Collapsed Lungs - are where the airways are fully closed due to the build-up of mucus in the airways, leading to a full plug being stuck in the airways, stopping air from entering and exiting the air sac. Because air can’t escape from the air sac, the lungs absorb the CO2 from the air sac through the blood stream and move it to another air sac which can then release this gas. The air sac remains collapsed and is no longer used.
- Obstruction in the Airways – The mucus builds up making it harder to breathe and creating what is called an unproductive cough, i.e. a cough which fails to bring up mucus or phlegm as the mucus is stuck in the lungs and can’t get to the throat to be coughed out effectively. This causes a build-up in pressure and may lead to damage of the air sac.
These 3 conditions not only affect an asthmatic’s ability to breathe but also reduces the effectiveness of the medication as more and more medication is either trapped in the mucus or can’t access the airways where it is needed the most.
Medication is used to relieve inflammation, but it can’t release the trapped air or the mucus plug which causes the air sac to remain blocked.
If left untreated, this can lead to a decrease in lung volume of up to 25 millilitres every year. This is equivalent to around 1 shot glass every year or around 4 shot glasses every 4 years.
So How Do You Remove the Mucus to help Improve Lung Capacity and Lung Function?
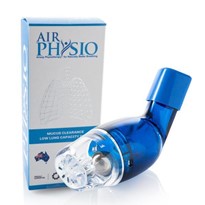
AirPhysio is an international award winning mechanical medical device which helps improve lung capacity and Lung function by doing the following:
- Mucus Removal and Clearance – The device shakes the airway walls (you can actually feel it working) and gets in behind the mucus and mucus plugs, helping to free it from the walls and start moving it up and out of the lungs to be swallowed or coughed out naturally.
- Lung Expansion – The device creates a positive pressure in the lungs and helps to open up closed and semi-closed airways, helping to restore lung capacity and maintain maximum lung capacity.
AirPhysio is an Australian Made and Owned Product, proudly partnered with Asthma Australia, is registered by the Therapeutic Goods Association (TGA) in Australia as a medical device in Australia and used in hospitals for patients with asthma to help asthmatics breathe easier, helping to improve effectiveness of medication when you need it most.
References
- National Heart, Lung and Blood Institute (n.d.). What is asthma? Retrieved from https://www.nhlbi.nih.gov/health/health-topics/topics/asthma/
- World Health Organization (n.d.). Chronic respiratory diseases: Retrieved from http://www.who.int/respiratory/asthma/en/
- Kudo, M., Ishigatsubo, Y. & Aoki, I. (2013). Pathology of asthma. Frontiers in Microbiology, 4(263), 1-16. doi:10.3389/fmicb.2013.00263.
- Lou, J., Liu, D., Chen, G., Liang, B., & Liu, C. (2017). Clinical roles of lung volumes detected by body plethysmography and helium dilution in asthmatic patients: A correlation and diagnosis analysis. Scientific Reports, 7, 1-9. doi:10.1038/srep40870.
- Lachowicz-Scroggins, M. E., Yuan, S., Kerr, S., Dunican, E. M., Yu, M., Carrington, S., & Fahy, J. (2016). Abnormalities in MUC5AC and MUC5B protein in airway mucus in asthma. American Journal of Respiratory and Critical Care Medicine, 194(10), 1296-1299.
- Athari, S. S., Athari, S. M., Beyzay, F., Movassaghi, M., Mortaz, E., & Taghavi, M. (2017). Critical role of toll-like receptors in pathophysiology of allergic asthma. European Journal of Pharmacology, 808, 21-27. doi:10.1016/j.ejphar.2016.11.047.
- Fanta, C. (1985). Clinical aspects of mucus and mucous plugging in asthma. Journal of Asthma, 22(6), 295-301. doi:10.3109/02770908509087113
- Fahy, J. V. & Dickey, B. F. (2010). Airway mucus function and dysfunction. The New England Journal of Medicine, 363(23), 2233-2247. doi:10.1056/NEJMra0910061.
- Maxwell, G. (2009). The problem of mucus plugging in children with asthma. Journal of Asthma, 22(3), 131-137. doi:10.3109/02770908509073131
- Witt, C. A., Sheshadri, A., Carlstrom, L., Tarsi, J., Kozlowski, J., Wilson, B.,… Castro, M. (2014). Longitudinal changes in airway remodeling and air trapping in severe asthma. Academic Radiology, 21(8): 986–993. doi:10.1016/j.acra.2014.05.001.
- Busacker, A., Newell, J. D., Keefe, T., Hoffman, E. A., Granroth, J. C., Castro, M.,… Wenzel, S. (2009). A multivariate analysis of risk factors for the air-trapping asthmatic phenotype as measured by quantitative CT analysis. Chest, 135(1), 48-56. doi:10.1378/chest.08-0049.
- Hartley, R. A., Barker, B. L., Newby, C., Pakkal, M., Baldi, M., Kajekar, R.,… Brightling, C. E. (2016). Relationship between lung function and quantitative computed tomographic parameters of airway remodeling, air trapping, and emphysema in patients with asthma and chronic obstructive pulmonary disease: A single-center study. Journal of Allergy and Clinical Immunology, 137(5), 1413-1422. doi:10.1016/j.jaci.2016.02.001
- Myers, T. (2007). Positive expiratory pressure and oscillatory positive expiratory pressure therapies. Respiratory Care, 52(10), 1308-1327
- Girard, J.P. & Terki, N. (1994). The flutter VRP1: a new personal pocket therapeutic device used as an adjunct to drug therapy in the management of bronchial asthma. Journal of Investigational Allergology & Clinical Immunology, 4(1), 23-7.
- Morsch, A.L., Amorim, M. M., Barbieri, A., Santoro, L. L., & Fernandes, A.L. (2008). Influence of oscillating positive expiratory pressure and the forced expiratory technique on sputum cell counts and quantity of induced sputum in patients with asthma or chronic obstructive pulmonary disease. Jornal Brasileiro De Pneumologia : Publicacao Oficial Da Sociedade Brasileira De Pneumologia E Tisilogia, 34(12), 1026-32.
- Samransamruajkit, R., Chin, T., Yuengsrigul, A., Newton, T., & Nussbaum, E. (2003). Possible beneficial effect of chest physical therapy in hospitalized asthmatic children. Pediatric Asthma, Allergy & Immunology, 16(4), 295-303.
- Swift, G.L., Rainer, T., Saran, R., Campbell, I. A., & Prescott, R. J. (1994). Use of flutter VRP1 in the management of patients with steroid-dependent asthma. Respiration, 61(3), 126-129.






-160x160-state_article-rel-cat.png)