Our lungs are amazing organs which help us breathe and exchange oxygen (O2) with carbon dioxide (CO2). This process is about removing excess carbon from our cells and blood which assist in balancing the acidity and alkalinity levels in our body, this helps us maintain pH level of 7.4 in our blood. This is also a similar ideal pH level of water and soil for growth.
This balance is maintained by 3 main organs working together to keep the balance. These 3 organs include the brain, heart and lungs. 2 independent parts of the brain work together, one to monitor oxygen levels in the blood and the other monitors the carbon dioxide levels.
If our blood has too much oxygen in the blood, the blood is alkaline and the lungs are told to stop taking a breath, as the carbon dioxide is allowed to build up. Too much carbon dioxide and the blood becomes acidic and the lungs are told to take a breath to remove the Carbon Dioxide from the lungs and breathe in more oxygen, while the heart is told to pump harder to gain more oxygen from the lungs.
The lungs are a semi automatic organ where we have the option to override these communication signals by holding our breath or breathing out excessively like blowing up a balloon until we become light headed. But in the end, these 2 parts of the brain help control the balance of pH levels by forcing you to take a breath when you hold it too long, or make you black out if you continue to exhale even when your carbon dioxide levels are too low, attempting to maintain a pH balance of the body.
What Happens When the Brain, Heart of Lungs Fail?
Poor Communication of the Brain
If either part of the brain has poor communication then it can lead to other symptoms related to the body becoming acidic or alkaline.
For example with a failure of communication with the part of the brain which monitors CO2 Levels. Have you ever noticed that when you are concentrating intensely for a period of time, you suddenly take a deep breath out of no where. This is the brain telling you to take the breath because your CO2 levels have reached a peak in your lungs. For someone with Central Sleep Apnea, this part of the brain may not function correctly and they start to turn blue, just sitting there.
For example with a failure of communication with the part of the brain which monitors O2 Levels. When you blow up too many balloons in a short period of time, you start to feel light headed and may black out if you don't stop. This is the brain telling you to stop breathing and telling you to allow the CO2 to build back up in your lungs. For someone who consistently blacks out, this may be caused by poor communication of this part of the brain.
Heart Failure
As most people know, the heart has 2 main steps as follows:
1. Collect oxygen from the lungs and deliver to the heart and distribute it to the rest of the body
2. Collection of carbon dioxide from the body and deliver the carbon dioxide to the lungs for expelling
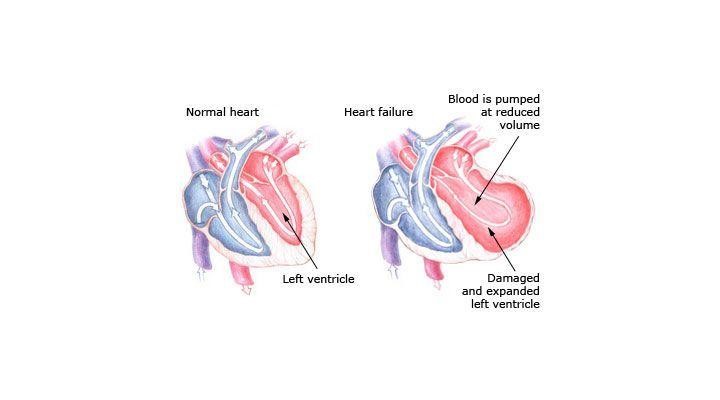
The right side of the heart collects the carbon dioxide from the body and then pump it to the lung to receive oxygen and then return the oxygenated blood to the left side of the heart to be distributed to the rest of the body.
If the right side fails, then the level of oxygen in the blood drops as there isn't enough blood being pumped to the lungs at a fast enough rate. This means that the oxygenated blood being delivered to the left side of the lungs is lower and it has more pressure to take most of the work of pumping around the body. This may lead to swelling (fluid build up) in the extremities like fingers, feet, etc... as there is a lower amount of oxygen being delivered, resulting in the cells becoming acidic and releasing more lactate, also known as lactic acid.
Respiratory Conditions
When the lungs are working correctly we have a simple process where our lungs excrete mucus (which captures up to 90% of all foreign particles) which sits on top of hairs known as cilia. This mucus is transported at around 1 centimetre per minute and is swallowed (we swallow around 30 millilitres per day). This process is called the mucociliary escalator and is responsible for helping to maintain the hygiene of our lungs.
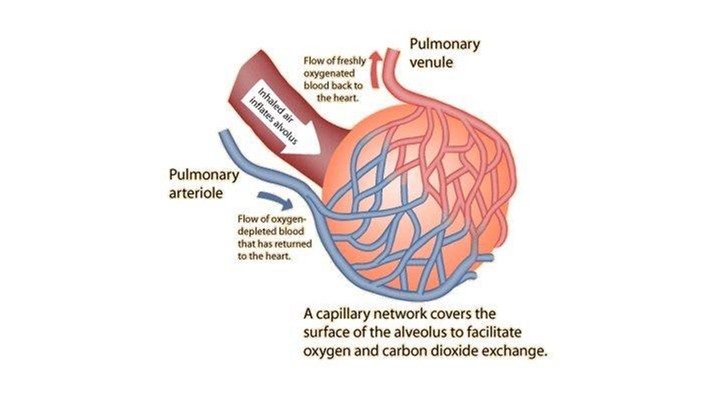
This process helps to filter our particles before they reach our alveoli (air sac) where the gas exchange of O2 and CO2 happen.
When we get an infection in our lungs, 2 important immune responses happen:
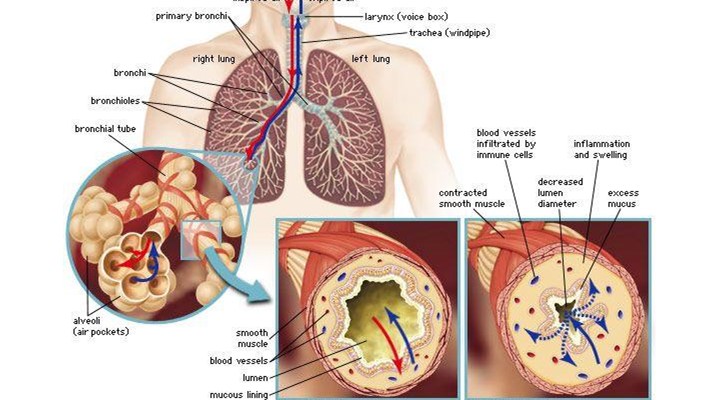
- Mucus Hyper Secretion and Mucociliary Escalator - The 1st line of lung defense which captures up to 90% of all foreign particles. This is where the airways secrete thicker mucus so as to capture and remove pollutants from the airways before they it reaches the airway walls.
- Inflammation of the Airway Walls - The 2nd line of lung defense. This occurs if any particles, bacteria or viruses make it through the mucus and enter the skin cells of the airway walls. In this case, the airway walls fill with blood and fluid as the white blood cells are pushed into the muscle to help fight infection. By filling with blood, the tissue expands, causing heat and pain, i.e. the inflammatory condition.
The only issue with these 2 conditions are that they restrict the amount of oxygen which reaches the alveoli (air sacs) which reduces the amount of oxygen in the blood. As a short term fix, the blood increases the amount of hemoglobin to assist in mitigating this. If this occurs long term (i.e. long term inflammation and/or mucus plugging), then it can result in an imbalance of O2 and CO2 in the body, resulting in the conditions mentioned above.
These Respiratory Conditions usually develop into 1 of the following:
1. Asthma - An immune deficiency conditions where the lungs react to a specific Alligen or parasite attack by creating mucus hyper secretion, inflammation and Bronchoconstriction (a condition where the muscles in the airways constrict to force the alligen/parasite out of the lungs
2. Acute Bronchitis or Chronic Bronchitis - A reaction to an infection of the lungs where the lungs react by mucus hyper secretion and/or inflammation. Chronic Bronchitis (also know as 1 condition of COPD) is from a long term condition of Bronchitis (usually 3 months or more) over a 3 year period.
3. Bronchiectasis - This is a condition where the cilia (airs on the airway walls) and/or airway walls are damages. This can occur from a thing TB or uncleared mucus from an infection over a long period, or even something as simple as old age. This leads to a damaged area of the mucociliary escalator where mucus pools in and starts to block the clearance process of the lungs, leading to further complications.
4. Cystic Fibrosis - This is a hereditary condition where the mucus which is sticky and thicker due to dehydration. This leads to an inability for the mucociliary escalator to work efficiently
The consistency of the mucus is essential for capturing of the particles and then being transported out of the lungs. If it is too dehydrated and thick, it slows the process and doesn't transport as easily creating blockages and inflections. If it is too hydrated and not sticky enough, it doesn't ride easily on top of the cilia (hairs) and may slide down onto the skin, making it harder to transport and causing further infections and inflammation.
Treatment of Inflammation and Mucus Hyper Secretion
The inflammation is usually treated through medical known as Corticosteroids, which the excess mucus is usually treated using either a PEP or OPEP device like AirPhysio. These devices expand the lungs when blowing out, helping air to get behind the mucus to assist in pushing it up and out of the lungs to be swallowed or coughed out naturally. They also help to splint open the airways and push medication further into the lungs, improving deposition.