Vaccines are particularly temperature sensitive and must be stored within strict temperature parameters to be safe and viable. The guidelines, also known as “Strive for 5”, were aptly named to give vaccine providers a memorable point of reference, with ‘5’ referring to the perfect vaccine storage temperature of +5°C. This is the midway point between the acceptable temperature range of +2°C and +8°C recommended in the national guidelines.
The National Vaccine Storage Guidelines help health providers safely manage vaccine temperatures during transport, storage and cold chain breaches. They specify the temperature range, the type of fridges required for vaccine storage, and assist with cold chain management and breach protocol. The guidelines were developed so that patients receive effective and potent vaccines from health services like medical practitioners, hospitals, clinics, mobile services and outreach providers.
What is the Cold Chain?
The ‘cold chain’ is the system of transporting and storing vaccines within the safe temperature range of +2°C to +8°C. This chain starts when the vaccine is manufactured, continues through to vaccine distribution centres and immunisation service providers, and ends when the vaccine is administered.
For the cold chain to remain unbroken, the temperatures are not allowed to go outside these two temperature parameters at any stage of the process. The National Storage Guidelines Strive for 5 promotes the best practices for safe storage of vaccines, ensuring that the cold chain remains unbroken.
What is a Cold Chain Breach?
A cold chain breach is when the vaccines are exposed to temperatures outside the recommended +2°C to +8°C. Vaccines are delicate biological substances that can be quickly destroyed if subjected to varying heat or cold outside the cold chain requirements. When a cold chain breach occurs, vaccines have been exposed to these temperatures for longer than 15 minutes, and are potentially unusable. All cold chain breaches must be reported to the Victorian Department of Health.
A cold chain breach may occur if there is a power outage. One way to protect vaccines from a cold chain breach in this situation is to invest in a Medical UPS battery backup. A UPS battery backup helps avoid a cold chain breach by keeping power connected to the refrigerator and ensuring temperature stability, even in unusual circumstances where no other back-up protocol can be actioned.
Why is Vaccine Storage Important?
Vaccines are an important part of eradicating or preventing common diseases. They must be stored and handled safely to ensure quality and usability to continue to protect the community. However, vaccines are also temperature sensitive and will not survive for long periods of time outside specific conditions.
The recommended temperature range for the safe storage and handling of vaccines is 2°C to +8°C. Storage or handling outside these parameters may reduce vaccine potency and risk patients receiving ineffective health products. The result could be inadequate immune responses from patients and lowered protection against disease. Apart from patient wellbeing, vaccines are expensive and can be in short supply. Vaccines that are not stored properly will have to be replaced which is a further financial cost.
Key Aspects of Vaccine Storage Management
Vaccine storage management helps ensure vaccines are stored within the recommended temperature range and the cold chain is maintained so that patients receive vaccines that are safe and effective. To help maintain appropriate vaccine storage guidelines, these key aspects must be followed:
-
Strict temperature control. Understanding the guidelines of strict temperature control is the first step in vaccine storage management. This means knowing that most vaccines must be stored in temperatures between +2°C to +8°C, and that any variance outside these temperatures may lead to the degradation of temperature sensitive medications.
-
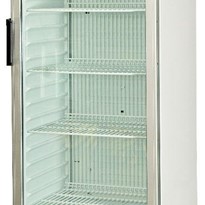
Store vaccines in a purpose-built medical fridge/freezer. Medical fridges and freezers designed for the safe storage of vaccines adhere to strict temperature guidelines of +2°C to +8°C. Health providers must store vaccines in purpose-built medical fridges or freezers rather than domestic fridges. Medical fridges provide a greater level of security and temperature control than normal fridges and are an essential piece of equipment for vaccine storage. Medical fridges ensure the safe storage of temperature sensitive medications with precision temperature control, reliable data logging, alarms, and temperature monitoring.
-
Vaccines must be protected from the light. Vaccines may lose potency if exposed to direct sunlight or ultraviolet light. For this reason, do not remove original cardboard packaging when storing vaccines in a refrigerator. The original cardboard packaging helps prevent exposure to sunlight or ultraviolet light, temperature fluctuations, possible breach of sterility, tampering, or vaccine administration errors.
-
Education and training. All staff must be educated on the importance of maintaining the cold chain in vaccine storage and handling. Any person who handles vaccines is responsible for maintaining the cold chain, from receptionists to laboratory technicians. Staff need to understand the importance of effective vaccine management and their role in ensuring the guidelines are adhered to. A staff member should be nominated to take responsibility for vaccine management, and a back-up staff member should be assigned in case of their absence.
-
Ensure policies and protocols are in place. An effective vaccine management protocol will ensure the health provider is ready before an emergency occurs. Vaccine management protocol should include written instructions on the protocol of vaccine ordering, vaccine delivery, temperature monitoring and recording, power outage and procedure, cold chain breach, documentation, equipment maintenance, and transporting vaccines offsite.
-
Report temperature outside cold chain requirements. When vaccines are exposed to temperatures outside the cold chain requirements of +2°C to +8°C, this is known as a cold chain breach and must be reported to the Department of Health. The standard process for cold chain breach reporting is:
*Complete the cold chain breach report form when vaccines have been exposed to temperatures greater than +8°C or less than +2°C for more than 15 minutes, or if vaccines have been exposed to light.
*Determine the length and extent of each breach.
*Download the data logger to assess the duration of the breach and extent of temperatures reached.
*Assess the Government funded vaccines that have been affected.
*Count the number of doses of each vaccine exposed.
*Review practice records to identify any vaccines exposed to a previous breach.
*Complete Cold Chain Breach report form and email to Health Department.
*Write a separate report for each vaccine affected and email to the immunisation department.
-
Vaccine storage self audits. Immunisation service providers are required to carry out a vaccine storage self audit at least once every 12 months, and more frequently if there have been problems with equipment or cold chain breaches. A self audit includes documenting safe handling and storage procedures, vaccine storage equipment, equipment monitoring, and alternative vaccine storage. A checklist is provided by the Health Department to make carrying out a self-audit as simple as possible.
Why is Vaccine Storage Management Important?
Vaccines are temperature sensitive and need a vaccine storage management plan to keep them safe and effective. The reasons vaccine storage management is important include:
-
Healthcare professionals have a responsibility to supply safe and effective vaccines that have not been affected by the heat or cold.
-
Vaccines are expensive and can be in short supply.
-
Vaccines with effective storage management protocols are likely to be effective and will preclude the need to revaccinate patients.
-
In well managed vaccine storage systems with effective procedures in place, it is more likely that problems will be detected and managed before vaccines become ineffective.
-
When vaccine storage is well managed it is a good quality assurance measure for an immunisation provider.
The National Vaccine Storage guidelines are in place to ensure vaccines remain safe and effective. These temperature sensitive medications require strict storage conditions within a temperature range of +2°C to +8°C. Any variation outside these conditions for more than 15 minutes is a cold chain breach. In this article we have explained how the vaccine storage guidelines are in place to help health providers avoid a cold chain breach and assure the safe delivery of vaccines to patients.




























(1)-205x205.jpg)













