Abstract.
– An outbreak of a novel coronavirus disease-19 (nCoV-19) infection began in December 2019 in Wuhan, China, and now involved the whole word. Several health workers have been infected in different countries. We report the case of a young man with documented nCoV 19 infection evaluated with lung ultrasound and discuss potential applications of lung ultrasound in this setting. Lung ultrasound allowed the identification of nCoV-19 infection at bed-side. Moreover, lung ultrasound can have several other advantages, such as reduced health worker exposition to infected patients, repeatability during follow-up, low-costs and easier application in low-resource settings.
Introduction
An outbreak of a novel coronavirus disease-19 (nCoV-19) infection began in December 2019 in Wuhan, China (1). Since then, nCoV-19 spread in 68 different countries in the world (including one cruise ship with 705 documented cases classified as “others”), causing 87.470 cases with 2.990 deaths as of March 1st, 2020 (https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6). The most common symptoms are fever and cough with a median incubation period of 4 days. The characteristic feature (and also the initial cluster observation that allowed the suspicion of a novel disease) is a development of pneumonia that, on chest computed tomography (CT), is seen as ground-glass opacity as main finding. Another characteristic feature is the frequent observation of lymphocytopenia (in 83.2% of the patients on admission)2.
Although the outbreak is not yet completely understood and in the last weeks there has been a huge amount of publications on the most important international journals, there are no reports yet on the possible use of lung ultrasound for the evaluation of patients with suspected nCoV-19 infection. Therefore, we report the case of a young man with documented nCoV-19 infection evaluated with lung ultrasound and discuss potential applications of lung ultrasound in the context of nCoV-19 outbreak.
Case Report
A 52 years-old-man was evaluated in our Emergency Department (ED) because of fever, cough, asthenia, headache, myalgia and photophobia since one week. He denied any travel during the last months, but reported a history of contact with several Chinese people (none with documented nCoV-19 infection) and Italian people coming from the City of Bergamo (Northern Italy), currently considered a high-risk area for nCoV-19 infection by the Italian Ministry of Health. His on-air oxygen saturation was 90% and low-flow oxygen therapy was started. On clinical examination, the man looked suffering and dyspneic, lung auscultation documented bilateral crackles. The remaining examination was unremarkable. Blood tests showed lymphocytopenia, thrombocytopenia, high LDH and inflammatory markers. Blood cultures were performed, and antibiotic therapy started. Chest X-ray showed a doubtful left peri-hylar hypodiafania (Figure 1). We also performed lung ultrasound. After these procedures, swab for respiratory viruses and nCoV-19 was performed and later resulted positive for nCoV-19.
Lung Ultrasound Technique
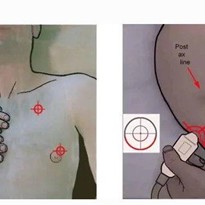
Lung ultrasound was performed with a portable convex probe (3.5 mHz), wireless-connected with a tablet. Such a device, despite providing
lower-quality images compared to last generation machines, was chose in order to minimize the risk of contamination of devices and subsequent nosocomial spread. Two operators, one ED physician (operator 1) and one ED nurse (operator 2), entered the isolation room respecting all the preventive measures for respiratory, droplet and contact isolation provided by the World Health Organization for the nCoV-19 outbreak. The ultrasound probe and the tablet were put in two different sterile, plastic probe and tablet covers (Figure 2a and 2b). Operator 1 performed lung ultrasound using the wireless probe and, therefore, entered in contact with the patient. Operator 2 held the tablet and was responsible to freeze and store images/videos, therefore did not touch neither the patient nor anything else within the
room. This procedure was shared and agreed by the two operators before entering the room, in order to minimize contamination risk due to the high-risk setting. At the end of the procedure, the tablet and probe were sterilized in a dedicated area and put into two new sterile plastic bags. The thorax was scanned in the following 12 lung areas at bed-side: anterior superior and inferior, lateral superior and inferior, posterior superior and inferior, bilaterally. Informed consent was obtained. In our Institution, the use of lung ultrasound is routinely included in the management of patients with respiratory conditions and approved by the Ethic Commitee. ID 2729
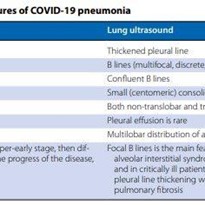
Lung Ultrasound Findings
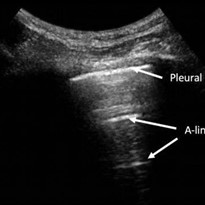
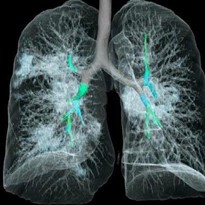
Lung ultrasound showed, on the anterior and posterior emi-thorax bilaterally, an irregular pleural line with small subpleural consolidations,
areas of white lung and thick, confluents and irregular vertical artifacts (B-lines) (Figure 3). Spared areas were present bilaterally, mixed with pathological areas. As a control-case, we report images made with the same device using the same ultrasound settings, performed during the same ED shift on a 38-years-old woman with high-grade fever, diffuse muscle and joint pain and cough, coming from a high-burden coronavirus area in Northern Italy, which eventually tested negative to nCov-19. Lung ultrasound showed a normal pleural line with A-lines regularly reverberating and only one, regular vertical artifact (B-line) noted in a single area (Figure 4).
Discussion
We provided the first lung ultrasound description of nCoV-19 pneumonia in a relatively young man with respiratory distress and confirmed etiological diagnosis. Lung ultrasound clearly documented signs suggestive for interstitial-alveolar damage3 showing bilateral, diffuse pleural line abnormalities, subpleural consolidations, white lung areas and thick, irregular vertical artifacts. The role of lung ultrasound to evaluate several respiratory conditions is nowadays widely documented. However, the use of lung ultrasound in the evaluation of a suspected or confirmed nCoV-19 patient (and in general during highrisk infectious disease outbreaks), particularly using pocket devices, has several implications. First of all, lung images can be obtained directly at bed-side by the same evaluating clinician, therefore reducing the number of health workers potentially exposed to the patient. Currently, the use of traditional imaging such as Chest X-Ray or CT scan require the patient to be moved to the radiology unit and potentially several people can be exposed, from health care professional to the other patients requiring later a CT scan for other reasons. Using lung ultrasound, the same evaluating clinician can visit the patient, perform blood tests or insert intravenous lines if required and obtain lung images with portable devices on the same time. This is a primary point since last data are clearly showing that, in most involved countries such as China and Italy, about 3 to 10% of infected patients are health workers and
hundreds of them are in quarantine, determining a serious problems of health professionals’ shortage. In most hospitals, this is generating problems in daily care of all patients (including non nCoV-19 patients) and most nurses/doctors are performing non-stop clinical rotations; also, some Italian regions are evaluating the need to call back to work retired physicians. Secondly, lung ultrasound can allow a first screening and discriminate low-risk patients (lung ultrasound-negative patients that can initially wait for second level imaging if clinically stable and, therefore, reducing the risk of nosocomial exposure) from higher-risk patients (such as those with abnormal lung ultrasound patterns), that might require second level imaging or even experimental therapies. Moreover, a recent study showed that the sensitivity of chest CT was greater than that of real time-PCR (98% vs. 71%, respectively, p<.001) in detecting nCoV-19 infection, maybe due to immature development of nucleic acid detection technology, low patient viral load or improper clinical sampling. The same authors suggested that chest CT might be used for screening for COVD-19 for patients with clinical and epidemiologic features compatible with COVID-19 infection particularly when RT-PCR testing is negative. However, routine use of CT scan has several obvious implications while lung ultrasound would be much easier to use as a screening tool. Third, portable devices are definitely easier to sterilize due to smaller surface areas. Fourth, lung ultrasound can be performed on bed-side. This means that, using portable machines, infected but relatively well-being patients that have been discharged could be evaluated both with clinical examination and lung imaging directly in their homes. This is an important point since many highly affected countries, such as Italy, are experiencing saturation of admission beds in many hospitals. Having this opportunity would allow a safer discharge of patients. Fifth advantage, although linked to point four, lung ultrasound is radiation free and can be performed every 12 to 24 hours and would allow a close monitor of clinical conditions and also detect very early change in lung involvement. This is an important point since a recent study showed that CT pathological findings were more frequent when CT was performed later during the disease, particularly more serious findings such as consolidations, bilateral and peripheral disease, greater total lung involvement, linear opacities, “crazy-paving” pattern and the “reverse halo” sign. Sixth, lung ultrasound can be easily performed in the outpatient setting allowing general practitioners a better evaluation of patients, currently overwhelmed by the nCoV-19 general fear and asking more and more advices by their general practitioners. This would also allow a better pre-triage to determine those patients
that should be sent to the hospital. Last, lung ultrasound is a cheap instrument that could be easily applied also in poor settings. Recently, the first nCoV-19 case have been described in sub-saharian Africa (Nigeria). In case of a massive spread in this setting, traditional imaging is much more difficult to be performed compared with lung ultrasound.
Conclusions
We suggest clinicians facing the nCoV-19 outbreak to use and evaluate the role of lung ultrasound in patients with nCoV-19. Moreover, we
suggested a safe procedure to perform lung ultrasound at bed-side minimizing the risk of contamination. Larger studies could provide useful and practice-changing information that, importantly, could be translated to the management of new emerging respiratory infection outbreaks with a high-risk of human-to-human transmission.